Health Impacts & Reporting
Approximately 17.3 million people live within one-half mile of oil and gas development in the U.S. Many, especially those in underserved and underrepresented communities, live near multiple sources of emissions. And more than three million children attend school within a half-mile of these facilities. Over the last decade, researchers have been studying how those who live, work, and play near these facilities can be impacted both physically and mentally.
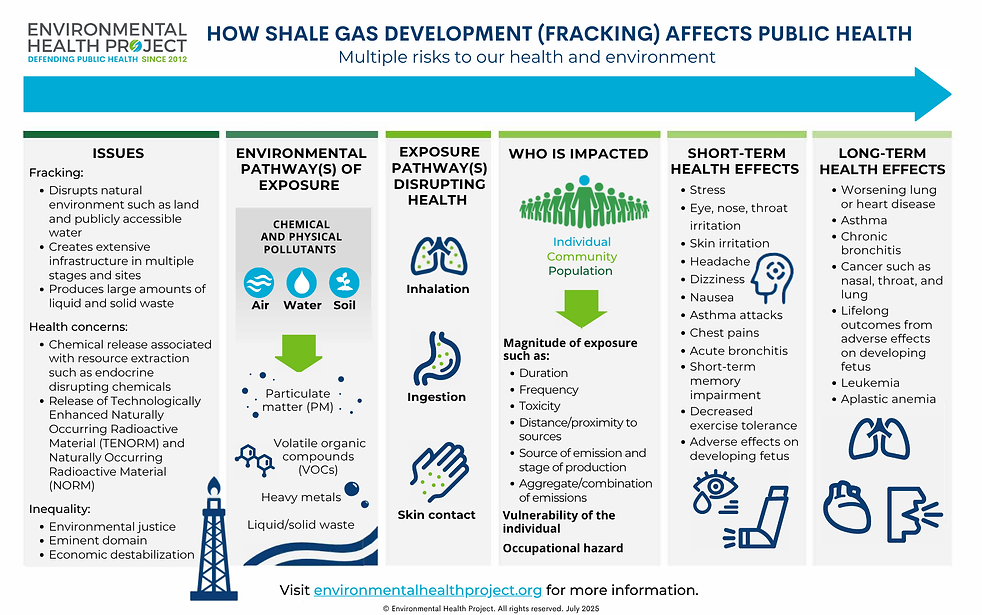
With respect to shale gas development (SGD) specifically, more than two dozen epidemiological studies have been conducted and show a correlation with poor health outcomes in people living in proximity to such infrastructure. These studies also indicate that health impacts increase the closer one is to shale gas facilities. Research indicates the following health symptoms are correlated with SGD:
-
Worsening or development of asthma
-
Babies born with congenital heart defects or neural tube defects
Stress, anxiety, depression, and other mental health symptoms also increase the closer one is to SGD. Stress in these environments tends to fall into one or more categories: physical stressors, psychological stressors, or psychosocial stressors. This could include things such as noise, light, and vibration disturbances, increased air emissions, and uncertainty or anxiety over the health of individuals and their families. For more information on how mental health or physical health is impacted please view our toolkit.
A question frequently asked is whether individuals living or working near SGD should undergo blood and urine testing (biomonitoring) to determine if they have been exposed to harmful chemicals from SGD. For more information on biomonitoring and when it is warranted check out our toolkit page.
For detailed information on known health impacts of chemical compounds associated with industrial operations, including oil and gas facilities, visit our Compounds of Concern tool. Compounds of Concern will be especially helpful to anyone living near polluting facilities. For example, if you are having trouble breathing and want to know what compound(s) may be causing that symptom, you can find possible answers here. Or, if you hear about the release of a chemical compound from a nearby facility in the news, you can find out more about what that compound is, how it’s used, and its related health effects.